 Guest Blog post by Marjan van den Akker, Academic Centre of General Practice, KU Leuven, Belgium.
Guest Blog post by Marjan van den Akker, Academic Centre of General Practice, KU Leuven, Belgium.
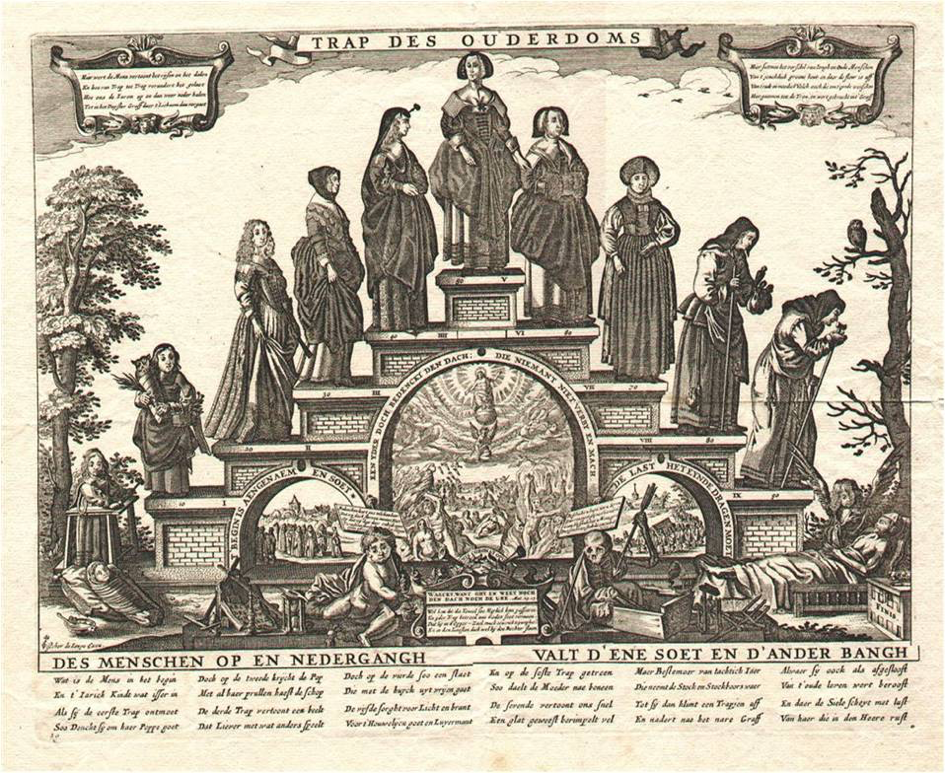
Multimorbidity – the co-occurrence of two or more chronic diseases(1) – and polypharmacy – the use of five or more chronic medications(2, 3) – are frequently described as the new epidemics of Westerns societies. In health care patients with multimorbidity and polypharmacy are the rule rather than the exception. Health care professionals are often overwhelmed by the complexity of those patients. Medical decision making is complex due to interacting treatments and diseases, and professionals find little support from the disease specific medical guidelines.
Looking at specific patterns of diseases and medications, the number of patients with specific combinations quickly drops. Therefore, the application of large datasets is inevitable to further fathom this phenomenon. Although coming from different countries, with diverse health care systems, large databases with medical information from different data sources are available in all Western countries. This can either be administrative data from health care insurers, or routinely collected data from primary care or from hospital medical files or discharge letters.
The INTEGO database, which covers over 2% of the Flemish population, is the only Belgian computerized morbidity registration based in general practice, containing coded diseases, medication prescriptions and lab results.
Within the context of MIDAS we have started to analyse patient trajectories of multimorbidity and polypharmacy. It would be of great interest to further extend those analyses using databases concerning socio-demographic information, such as people’s educational / socio-economic level and linking those to database comprising electronic medical records.
Despite the fact that multimorbidity and polypharmacy are well-known as highly relevant for the ageing population, its prevalence and incidence are also strongly on the rise in the middle aged populations, especially among people with a lower socio-economic class, who might start their disease trajectories up to an average of 10 to 15 years earlier as compared to their more affluent peers. Furthermore, health trajectories are not independent trajectories: there are influenced by medical management, but also by patients’ environment, life styles, and contextual factors.
Also, attention should be paid to the analyses of different birth cohorts, as there are serious indications that the patterns and trajectories of morbidity and medication are changing over time. Furthermore, comparing similar analyses using data from different countries helps to gain insight into the health inequalities within the European region.
This can help to identify vulnerable patient groups in more detail and clarify medication prescription patterns and provide suggestions for improving medical management and care for complex patients. Also, this information will help to guide health policy decision making for primary and secondary health care, as well as for public health strategies.
References
Truyers, C., Goderis, G., Dewitte, H., van den Akker, M., & Buntinx, F. (2014). The Intego database: background, methods and basic results of a Flemish general practice-based continuous morbidity registration project. BMC Med Inform Decis Mak, 14, 48. doi:10.1186/1472-6947-14-48
Muth, C., van den Akker, M., Blom, J. W., Mallen, C. D., Rochon, J., Schellevis, F. G., . . . Glasziou, P. P. (2014). The Ariadne principles: how to handle multimorbidity in primary care consultations. BMC Med, 12, 223. doi:10.1186/s12916-014-0223-1
Barnett, K., Mercer, S., Norbury, M., Watt, G., Wyke, S., & Guthrie, B. (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet, 379.
Canizares, M., Hogg-Johnson, S., Gignac, M. A. M., Glazier, R. H., & Badley, E. M. (2017). Increasing Trajectories of Multimorbidity Over Time: Birth Cohort Differences and the Role of Changes in Obesity and Income. J Gerontol B Psychol Sci Soc Sci. doi:10.1093/geronb/gbx004.
